
Introduction: The Complex Reality of HS Management
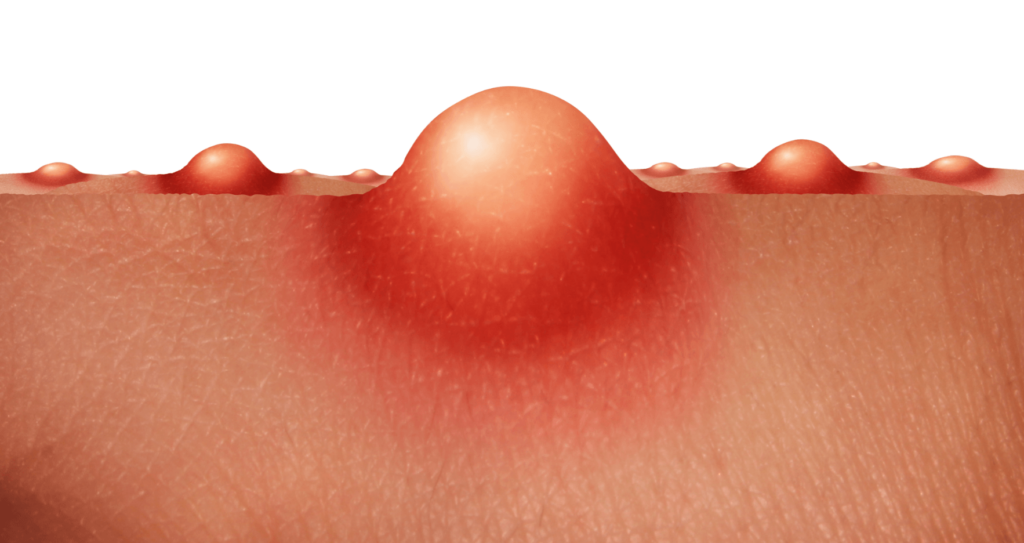
Hidradenitis suppurativa (HS) is more than just a skin condition—it’s a chronic inflammatory disorder that creates painful, recurrent abscesses and tunnels under the skin, primarily in sensitive areas like the armpits, groin, and under the breasts. For patients, HS isn’t just physically debilitating; it’s emotionally exhausting, often leading to social isolation, depression, and a diminished quality of life.
Why Personalised Care Matters in HS
- No “one-size-fits-all” solution – What works for one patient may fail for another.
- Treatment adherence is low – Many patients give up due to side effects or lack of results.
- Delayed diagnosis worsens outcomes – HS is frequently misdiagnosed as acne or boils, leading to years of ineffective treatment.
Recent research, including the THESEUS study and investigations into patient decision aids (PDAs), confirms that personalised, patient-centred approaches significantly improve outcomes. This article explores how HS treatment should be tailored—not just to the disease, but to the individual’s lifestyle, beliefs, and

Understanding Patient Preferences in HS Treatment
What Influences a Patient’s Treatment Choice?
HS patients weigh multiple factors when deciding on therapy, including:
1. Past Treatment Experiences
- “I tried antibiotics, but they ruined my gut.”
Many patients have negative experiences with long-term antibiotics (e.g., doxycycline, clindamycin/rifampicin), which can cause digestive issues, yeast infections, or antibiotic resistance. - “Surgery left me with worse scars.”
Some surgical interventions (e.g., deroofing, excision) may lead to slow healing or recurrence, making patients hesitant to try them again.
2. Healthcare Provider Recommendations
- Trust in the dermatologist’s expertise is critical.
- Patients are more likely to adhere to treatments if they feel their doctor understands their pain and lifestyle constraints.
3. Personal Beliefs & Lifestyle Factors
- “I can’t injections.”
Biologics (e.g., adalimumab) require regular dosing, which may not suit everyone. - “I prefer natural remedies first.”
Some patients want to avoid pharmaceuticals and explore diet changes, turmeric supplements, or topical CBD oil before stronger treatments.
What Does the Research Say?
- THESEUS Study Findings
- Patients reported high variability in treatment success.
- Laser therapy helped some, while others saw better results with surgery or biologics.
- Wound care struggles were a major post-surgical challenge.
- European Discrete Choice Experiment
- Effectiveness (47.9% priority): Patients want treatments that reduce flare-ups by 75-100% (not just 50%, the typical clinical trial benchmark).
- Pain reduction (17.3% priority): HS is excruciating—patients prioritise therapies that lower pain quickly.
Key Takeaway: HS treatment must be customised based on patient history, daily life, and desired outcomes—not just clinical guidelines.
The Challenges of Personalised HS Care (And How to Fix Them)
Barrier 1: Delayed & Fragmented Care
- Problem: Many HS patients wait years for a proper diagnosis. Even after diagnosis, access to specialised treatments (e.g., biologics, laser therapy) is limited.
- Solution:
- Fast-track referral pathways for suspected HS cases.
- Multidisciplinary clinics (dermatology + surgery + wound care) to streamline care.
Barrier 2: Poor Patient-Doctor Communication
- Problem: Patients often forget or misunderstand treatment discussions due to stress, pain, or time gaps.
- Solution:
- Use visual aids (e.g., diagrams of surgical options).
- Provide written summaries after consultations.
- Adopt HS-specific Patient Decision Aids (PDAs)—these improve knowledge and reduce anxiety.
Barrier 3: Psychosocial & Financial Struggles
- Problem: HS leads to depression, unemployment, and financial strain (due to costly dressings, missed work).
- Solution:
- Integrate mental health support (CBT, support groups).
- Advocate for insurance coverage of HS treatments.
- High Cost: Laser ablation and dressing is expensive and the cost of biologic therapy is often not affordable.
A Step-by-Step Personalised HS Treatment Plan
Step 1: Comprehensive Assessment
- Medical History: Previous treatments, allergies, comorbidities (e.g., PCOS, diabetes).
- Disease Severity: Hurley staging (I-III) + patient-reported pain levels.
- Lifestyle Factors: Work schedule, diet, stress levels.
Step 2: Shared Decision-Making
- Option 1: Medical Therapy
- Mild HS: Topical clindamycin + zinc supplements.
- Moderate-Severe HS: Biologics (adalimumab) or oral anti-androgens (spironolactone).
- Option 2: Procedural/Surgical
- Laser (Nd:YAG): Reduces inflammation in early-stage HS.
- Deroofing: For recurrent sinus tracts—less scarring than excision.
- Option 3: Integrative Approaches
- Diet modifications (low-glycemic, dairy-free).
- Stress management (yoga, mindfulness).
Step 3: Ongoing Support & Adjustments
- Monthly follow-ups to track progress.
- Wound care coaching for post-surgical patients.
- Pain management strategies (lidocaine patches, nerve blocks).
Conclusion: HS Care Should Be as Unique as the Patient
HS is a lifelong battle, but with personalised, patient-driven care, remission is possible. The best outcomes come from:
✔ Listening to patient experiences
✔ Offering flexible treatment options
✔ Addressing emotional & financial burdens
Take Control of Your HS Journey
At The Skincare Network, we specialise in bespoke HS management—because your treatment should fit your life, not the other way around.
📅 Book a Personalised HS Consultation Today:
🌐 www.skincarenetwork.co.uk
