
Malignant melanoma is thankfully rare in children, so research on substantial numbers of current patients is not feasible. A study in 2017 did look at cases over a 35 year period, to give a reliable view.
This was partly undertaken as other research had suggested a notable increase in paediatric melanoma. A study later the same year confirmed this, identifying an almost 150% increase over the previous four decades.
In the 35 year study, there was a nominally higher incidence in boys than girls but the split could be regarded as equal. As with other studies, areas of the body affected were also consistent.
They were parts with high exposure to the sun, the trunk, hands, arms, lower legs and feet, along with children’s eyes.
Around 10% of the studied cases were melanoma in the eye, higher than the adult incidence. A reminder that young eyes are vulnerable and of the value in having them covered by wrap around sunglasses.
The study timing meant some cases being to recent to include when considering outcome, although the longer term gave a clear picture:
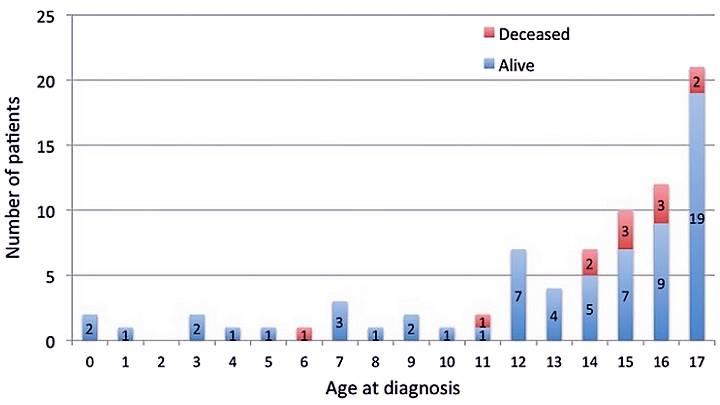
The 10 year mortality rate was 15%. High for any childhood disease and a significant reason for this became evident in the data.
Missed Opportunity
Whilst the melanoma may have existed earlier, correct diagnosis typically took place in teenage years. A time when melanoma is more likely to look similar to the condition seen in adults.
Initial opportunities may have been missed, due to lack of awareness, or specialist knowledge. With the stage at time of diagnosis such a key factor, this can mean no cure, or greater intervention to bring one.
Early stage melanoma is often cured in adults with surgical excision alone. The principle applies in children but with the higher number of late stage cases, there was more need for
chemotherapy and/or radiotherapy.
That children get a range of skin conditions is appreciated but if they uncommon, they should be seen by a specialist dermatologist. The same makes sense for unusual changes in moles, or lesions.
Paediatric Risk Factors
A further piece of research in 2017 looked at diagnosis, treatment and prevention of paediatric melanoma, with understanding risk factors a core component.
They found that only 22% of cases had predictable factors, such as fair skin, family history, genetically linked conditions, or pronounced nevi patterns.
These are still important, familial factors, extra large moles, or high numbers of moles in childhood make a substantial difference. Children with over 100 moles are 15 times more likely to see melanoma than those with around 10 moles.
Other complications such as immunosuppression, or rare birthmarks matter. The whole list of added risk factors does call for extra support, they are simply being numerically overwhelmed by another cause.
Exposure To The Sun
Paediatric melanoma accounts for almost 10% of all cancers seen in 15 to 19 year olds. As mentioned, this can be advanced, with serious consequences, yet in almost all cases is entirely avoidable.
Protecting children from too much sun exposure is not easy but can be done. Early adoption of practices such as sunscreen and protective clothing help at the time and make a difference to them becoming habitual.
The next most important early decision comes when something unusual is found on a child’s skin. Wherever you are, finding a specialist dermatologist with knowledge of paediatric skin conditions is a valuable step.
Peace of mind can follow and if required, children’s skin cancer treatment is often minimal for initial stage cases. Research on childhood melanoma points to two clear requirements, protect the skin and if a problem develops, diagnose as soon as possible.
