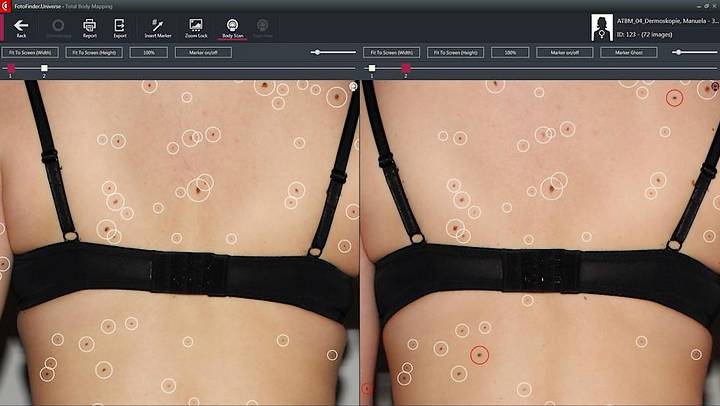
 Modern digital imaging coupled with specialist software helps to locate quite small changes in our skin over time.
Modern digital imaging coupled with specialist software helps to locate quite small changes in our skin over time.
Total body photography (TBP) is a term often used in dermatology, although others such as full body photography have the same meaning. Mole mapping is perhaps better known and is a specific use of TBP.
The objective of all dermatological body photography is to map change in lesions and identify new ones, through sequential imaging. Areas of concern can be examined by a consultant, helping to detect early stage skin cancers.
The incidence of skin cancers in general and malignant melanoma in particular has risen significantly in recent decades, with early detection remaining the key factor in reducing treatment and saving lives.
Logic suggests that total body photography should be valuable in skin cancer screening and individual studies appear to confirm this. In early 2021, a group of researchers pulled together data from a number of sources, to establish a wider picture.
They chose 14 studies, carried out in Europe, Australia and the US, representing the outcomes of over 12,000 patients. Their focus was on melanoma detection, along with the severity of tumours when detected.
Core Findings
In overall terms, detection through TBP improved, compared to standard approaches. The difference in stage of detection was particularly notable.
This was measured using Breslow thickness, a method of establishing the depth of a melanoma, from the skin surface to the base of the tumour. Compared to general data, TBP detected melanomas were at a 30% less invasive stage.
Alongside detection of change at an earlier stage, TBP showed an ability to identify malignant growths which were new arrivals. A combination which can mean less treatment, often cure by surgery alone and lower mortality.
Applying The Benefits
Thinner tumours boost survival rates for everyone, so should everyone have regular total body photography. In an ideal world they should and we would encourage anyone who wished to take part but on a national health service basis, cost factors matter.
TBP has been made more or less available nationally in Germany and to a lesser extent Australia but most health services baulk at the spend.
The core need is to improve targeting, by better understanding risk factors. For melanoma, family history, previous incidence, a large number of moles, or clinically atypical moles would be seen as factors but what about having fair skin.
You could potentially add in age, immune issues, perhaps more. Risks identified in the reports the researchers looked at were quite diverse. The conclusion was a need to harmonise risk prediction tools and improve the criteria.
We are pleased to offer an effective form of screening to our patients but to be available nationally, targets would need to tightly honed.
Targeted Improvement
More recent research has proven that TBP can improve early detection of melanoma in high risk populations. All good dermatology clinics should identify people who would particularly benefit and tailor screening to their needs.
Our clinic uses the latest systems but these can also be improved. Specialist software currently assists and fresh developments in artificial intelligence will see this aspect take skin cancer screening further forward.
The growth of 3-D screening may do the same, along with further research into body imaging. The need for an experienced consultant will always be there but advantages are evident in using the right technology to assist them.
You may find the options below useful:
- Save time with an intuitive search on: Skin Cancer Diagnosis & Treatment.
- Up to date news, research and insights: Our Dedicated Skin Cancer Blog.
For any advice, or to arrange a dermatology appointment, call 020 8441 1043, or send an email via the Make An Appointment button below.
